If you’ve ever noticed red bumps in your genital area after shaving, you may have wondered: are these just razor bumps, or could they be something more serious like a sexually transmitted disease (STD)?
While both conditions can cause similar-
bumps, they have key differences that can help you determine what’s really going on. Understanding these differences is crucial for proper treatment and peace of mind.
What Are Razor Bumps?
Razor bumps, also known as pseudofolliculitis barbae, occur when shaved hairs curl back into the skin, leading to irritation, inflammation, and small bumps. They’re common in areas with coarse or curly hair, such as the pubic region, underarms, and face.
Common Symptoms of Razor Bumps
Razor bump symptoms usually include:
- Small, red, itchy, or tender bumps
- Often appear shortly after shaving
- Found only in areas where hair was removed
- May contain pus if inflamed
Causes and Risk Factors of Razor Bumps
Razor bumps typically develop when hair follicles become irritated after shaving, often due to improper techniques or hair texture. Several factors contribute to their formation, including:
- Frequent Shaving with a Dull Razor: Shaving too often without giving the skin time to heal, especially with a dull blade, increases irritation and the risk of ingrown hairs.
- Curly or Coarse Hair: Naturally curly or coarse hair is more likely to grow back into the skin, leading to inflammation and razor bumps.
- Dry Shaving or Shaving Against the Grain: Shaving without proper lubrication or going against the natural direction of hair growth creates friction and increases the likelihood of irritation.
- Harsh Skincare Products: Aftershaves or shaving creams with alcohol, artificial fragrances, or harsh chemicals can dry out and irritate the skin, making razor bumps worse.
Razor Bumps Treatment
Most razor bumps heal on their own, but there are ways to speed up the process and reduce irritation. Avoid shaving for a few days to allow the skin to recover, and apply a warm compress to soothe inflammation and provide some razor bump relief.
Use a gentle exfoliant to help prevent ingrown hairs and moisturize with soothing products like aloe vera or tea tree oil can keep the skin hydrated and promote healing.
What Are Common STDs That Cause Bumps?
Being familiar with which sexually transmitted diseases or infections can cause bumps can help you determine if you have razor bumps or an STD. These STDs and STIs include:¹
1. Herpes (HSV-1 & HSV-2)
Herpes causes painful, fluid-filled blisters that eventually burst and form ulcers. These sores often appear in clusters and may cause itching, burning, or discomfort, sometimes accompanied by flu-like symptoms. While there is no cure, antiviral medications can help manage outbreaks and reduce transmission.
2. Genital Warts (HPV)
Genital warts are flesh-colored, cauliflower-like growths that develop in the genital or anal area. They are usually painless but can cause itching, discomfort, or minor bleeding if irritated. These warts are caused by certain strains of the human papillomavirus (HPV), and while they can be treated, the virus itself remains in the body.
3. Syphilis (Primary Stage)
Syphilis begins as a single, painless sore (chancre) at the site of infection, usually appearing within a few weeks of exposure. The sore heals on its own, but if left untreated, the infection progresses to more serious stages that can affect multiple organs. Early diagnosis and antibiotic treatment are essential to prevent long-term complications.
4. Molluscum Contagiosum
Molluscum contagiosum causes small, round, pearly bumps with a dimple in the center that may be itchy but are usually painless. The virus spreads through direct skin-to-skin contact and is sometimes classified as an STD when found in the genital area. Though the condition often resolves on its own, treatment can help speed up recovery and prevent further spread.
5. Scabies
Scabies is caused by tiny mites that burrow into the skin, leading to intense itching and a pimple-like rash. The infection spreads through prolonged skin-to-skin contact, including sexual activity, making it common among close partners. Prescription creams and medications are required to kill the mites and prevent reinfestation.
6. Chancroid
Chancroid is a bacterial infection that causes painful, soft sores in the genital area, often accompanied by swollen lymph nodes in the groin. Unlike syphilis sores, which are painless, chancroid ulcers are tender and can become larger or more inflamed if left untreated. Antibiotic treatment can effectively clear the infection and prevent complications.
Is It Razor Bumps or an STD? Main Differences
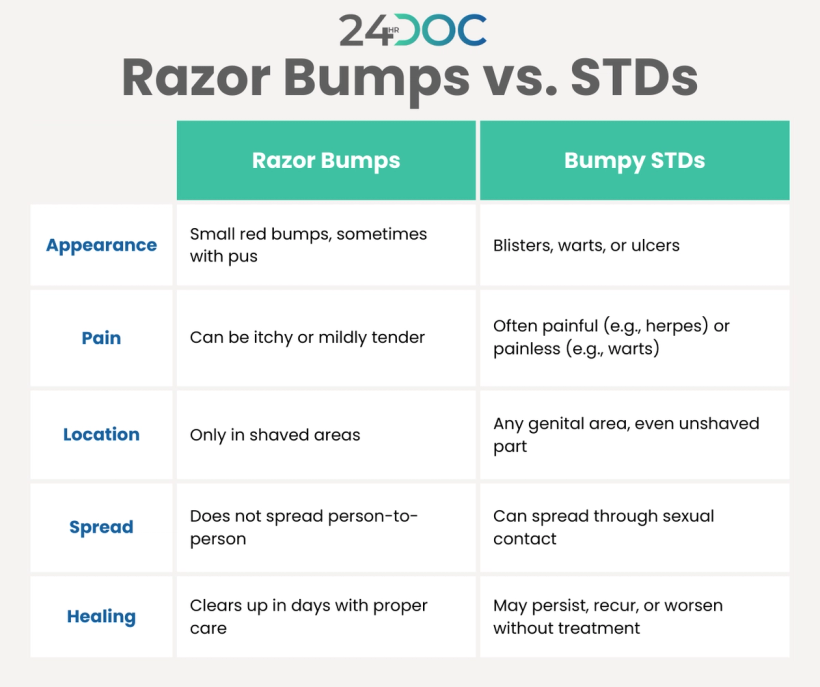
Razor bumps and sexually transmitted diseases (STDs) can sometimes appear similar, but key differences can help distinguish them. Razor bumps are small, red, and sometimes pus-filled, typically appearing in shaved areas. They are usually mildly tender or itchy, remain closed, and have a smooth surface, but they do not spread from person to person.
In contrast, STD-related bumps can vary in appearance, sometimes forming blisters, warts, or ulcers. They may be painful (such as herpes sores) or painless (like genital warts) and can be open or closed with a smooth or jagged edge, depending on the infection. Unlike razor bumps, which are confined to shaved areas, STD-related bumps can appear anywhere in the genital region, including unshaved areas.
STDs may cause other symptoms such as fever, headache, or swollen lymph nodes, while razor bumps are typically localized skin irritations. Razor bumps usually heal on their own within a few days with proper care, while STD-related sores may persist, worsen, or recur without treatment. Comparing the characteristics of razor bumps vs. STDs can help you determine which you have, but only a medical professional can determine with certainty.

When to See a Doctor of Genital Bumps
While shaving bumps on the genital area are usually harmless and self-resolving, certain signs indicate you should seek medical advice:
- The bumps last more than two weeks without improvement
- You experience additional symptoms such as pain, burning, itching, or unusual discharge
- The bumps appear after sexual contact or are spreading to other areas
- You have a history of STDs and are concerned about a recurrenc
A healthcare provider can examine the bumps and perform necessary tests to provide a clear diagnosis.
Frequently Asked Questions
Is it OK to squeeze razor bumps?
No, squeezing razor bumps can worsen inflammation, increase the risk of infection, and cause scarring. Instead, apply a warm compress and keep the area clean.
What is commonly mistaken for an STD?
Razor bumps, ingrown hairs, and skin conditions like folliculitis or molluscum contagiosum are often mistaken for STDs due to their similar appearance.
What is the difference between razor bumps and herpes?
Razor bumps are small, red, and confined to shaved areas, while herpes sores are painful, fluid-filled blisters that can appear anywhere in the genital region and may return in outbreaks.
What do shaving bumps look like?
Shaving bumps are small, red, and sometimes pus-filled. They typically appear in shaved areas and may be itchy or mildly tender. Infected razor bumps can become larger, more painful, and filled with pus, requiring proper care to prevent further irritation.
Know for Sure—Get Treated with 24hrdoc
If you’re unsure whether you have shaving bumps or an STD, getting a professional opinion can give you peace of mind.
At 24hrdoc, we make it easy to get fast, confidential online STD testing and treatment from the comfort of your home. Our licensed medical professionals can assess your symptoms, provide an accurate diagnosis, and prescribe treatment if needed—all without the hassle of an in-person visit
Don’t let uncertainty or embarrassment keep you from getting the care you need. Explore 24hrdoc today for discreet, reliable STD treatment and expert medical guidance.
Source: Medical NewsToday. What to know about sexually transmitted infections.




